Engineering Through COVID-19
A special report on the Rensselaer quest to combat the global pandemic.
Written by Strategic Communications and External Relations Staff
A mysterious respiratory illness first identified in Wuhan, China, in December 2019 began to make headlines in January 2020. The illness appeared first in an individual, then a small cluster of individuals. By March, it was all over the world. What was this mysterious disease? How was it spreading so rapidly and what could we do to stop it?
SARS-CoV-2 is a new strain of coronavirus that causes coronavirus disease, or COVID-19. Coronaviruses have been around for a long time. This virulent new strain, however, was different, vicious. “The virus, for which there is no therapy, enters the eyes, nose, or mouth and takes hold in the airways of the exposed person by binding to angiotensin 2 receptors in the airway,” says Dr. Anthony Szema ’86, an allergist, immunologist, and pulmonologist. “The lungs become inflamed so that there is ineffective gas transfer. That is why for the most severely affected, lack of oxygen in the blood or hypoxemia requires mechanical ventilation.”
And ventilation can be risky, Szema says. Among the patients who were ventilated early in the pandemic, there was an 88% mortality rate. In China, thousands of physicians contracted coronavirus. “High risk occurs during intubation because of exposure to infected secretions in the airway. For that reason, personal protective equipment, or PPE, is important.”
What began as a handful of cases at the beginning of the year skyrocketed to more than 3.3 million cases worldwide and over 237,000 deaths as of May 1. As the numbers continued to climb, life as we knew it came to a screeching halt.
COVID-19 impacted every part of society. Hospitals were quickly overwhelmed, and experienced shortages of ventilators and PPE. Schools and non-essential businesses closed. In hot spots all over the world, the number of cases grew exponentially by the hour.
When the governor of New York enacted NY PAUSE, Rensselaer quickly pivoted to remote instruction for the spring semester. COVID-19 was incorporated into the curriculum in numerous ways, including modeling its transmission and infectious disease spread, examining its impact on electricity consumption and forecasting, studying sterilization using deep UV LEDs, and challenging students to devise solutions.
As social distancing became the new normal, researchers shifted their work to help to fight the virus and mitigate the impacts of the pandemic. COVID-19 had become our most immediate and pressing challenge.
Data Matters
“Dealing with COVID-19 is a ‘big data’ problem, and artificial intelligence (AI) is a crucial tool in the big data toolkit.” According to James Hendler, the Tetherless World Professor of Computer, Web, and Cognitive Sciences, “A key challenge of using data analytics on complex real-world problems like the COVID- 19 pandemic is that finding solutions requires the combination of expertise from people who understand the problems — in this case, epidemiology and virology — and those who can understand how to use the data modeling and computational technologies needed to attack them.”
To further aid in the fight, Rensselaer offered governments and researchers from other institutions access to AiMOS, the Artificial Intelligence Multiprocessing Optimized System (Here's everything you need to know about it). As part of the COVID-19 High Performance Computing Consortium that was announced by the White House March 23, Rensselaer is working with researchers to use the supercomputing power of AiMOS to answer questions about the spread of the virus over time and its effects, explore potential vaccines and treatments, and analyze materials that could be used for PPE.
“In order to combat the devastating effects of this pandemic, we must be able to fully grasp the complexities and interconnectedness of biological systems and epidemiological data, as researchers work to develop therapeutic interventions and address gaps in our knowledge,” says President Shirley Ann Jackson.

“This effort requires expertise, collaboration, and the ability to process incredible amounts of data. Rensselaer offered all three at this critical time. In particular, the ability to model at very large scales which requires the unique capabilities of AiMOS,” she says.
AiMOS is able to perform eight quadrillion calculations per second, speeding the time for researchers to determine solutions that could ultimately save lives. According to Chris Carothers, director of the Center for Computational Innovations, Cleveland Clinic is seizing the power of AiMOS in a massive hunt for an existing drug to defeat the virus. Using a systems pharmacology-based network medicine platform, information on how drugs interact with human biology at the molecular level is being combined with information on how the virus attacks cells. Researchers are looking for potential interactions between drug activity and the virus’s offensive playbook. A high confidence match could be a good drug candidate for further exploration.
“AI and data analytics can be crucial tools in helping us to not just model the virus at a molecular level, but also to identify what medical procedures can work best for which population,” says Hendler, who is also director of the Institute for Data Exploration and Applications (IDEA). “In addition, they also allow us to explore how to not just predict, but also mitigate, the spread of this major pandemic. Scaling these techniques using the power of AiMOS allows us to work on these problems on a large scale, exploring solutions not just at a local scale, but also globally.”
Kristin Bennett, associate director of IDEA and professor of mathematical sciences, examines how and why COVID-19 impacts regions differently. Using the MortalityMinder, a data visualization tool developed by Bennett and her students in 2019, the team created COVIDMinder. The tool uses daily updated data to compare community risks, mediation tools, and outcomes related to COVID-19 by state across the U.S., and by county within New York state.
“Your community directly affects your health outcomes, and we’re seeing that play out in the COVID-19 pandemic,” says Bennett.
The initial version of the COVIDMinder allows users to view visualizations showing disparities in COVID-19 mortality rates, testing, hospital beds, and other key factors by state. For New York, data is also available by county. Bennett and her team are expanding COVIDMinder by adding new views and factors to help states and counties understand and combat the pandemic regionally. It can be accessed at covidminder.idea.rpi.edu.
As new epicenters emerge in densely populated cities, the virus gained a foothold in smaller communities. Researcher Malik Magdon-Ismail employed machine learning to model the pandemic’s impact across various scenarios in smaller cities. Using county data available through the New York State Department of Health and machine learning, Magdon-Ismail developed a predictive model that can determine local aspects of the pandemic such as the rate of infections over time, the infectious force of the pandemic, the rate at which mild infections become serious, and estimates for asymptomatic infections.
“These models show that the projections vary enormously from one city to another. This knowledge could relieve some of the uncertainty that is around in developing policy,” says Magdon-Ismail, professor of computer science.
Modeling smaller cities with machine learning is a challenge. Since few data points are available and they are updated less frequently than data on the nation as a whole or an epicenter, generic machine learning using such data would likely produce inaccurate predictions.
Magdon-Ismail was able to look at scenarios involving the practice of social distancing to predict the pandemic’s peak. “This kind of modeling is exactly what we need to know,” says Curt Breneman, dean of the School of Science. “That’s the power of modeling like this — you can actually ask, What if?”
Everyone talks about flattening the curve, but which curve? The models vary depending on social distancing factors and the data. We need to be cautious about returning to “normal” too quickly, Breneman says, before there is a good treatment or preventive measure available. “We really don’t know how good those projections are until we see the data.
“Data is where science gets to shine,” Breneman continues. “It may not always tell you the exact thing you need to know, but it will tell you where to go, where not to go, and where the most important discoveries are yet to be made.”
Pursuing Prevention and Treatment
While data is central to the pandemic solution, new interventional therapeutics are necessary to prevent new infections, create solutions to save lives, and provide a vital hedge against the growing threat of global pandemics.
One promising strategy comes from a team that has been pursuing a potentially powerful solution to pandemic control: a “viral trap” that is easily adapted to different classes of viruses, enabling a novel approach to virus detection and antiviral activity.
Jonathan Dordick, the Howard P. Isermann Professor of Chemical and Biological Engineering, and Robert Linhardt, the Ann and John H. Broadbent Jr. ’59 Senior Constellation Chair in Biocatalysis and Metabolic Engineering, have been exploring how their work in the areas of viral detection, therapy, and inhibition could be used against COVID-19 and other viruses in the future.
The viral trap they developed is a DNA-based nanotechnology designed to capture and kill viruses floating in the bloodstream. In previous research on the dengue virus, the team developed the world’s most sensitive test for dengue, and a novel means of capturing and ultimately killing the virus. Due to its design, the viral trap is adaptable to a range of viruses, according to Dordick, whose team also demonstrated the same approach for influenza A.
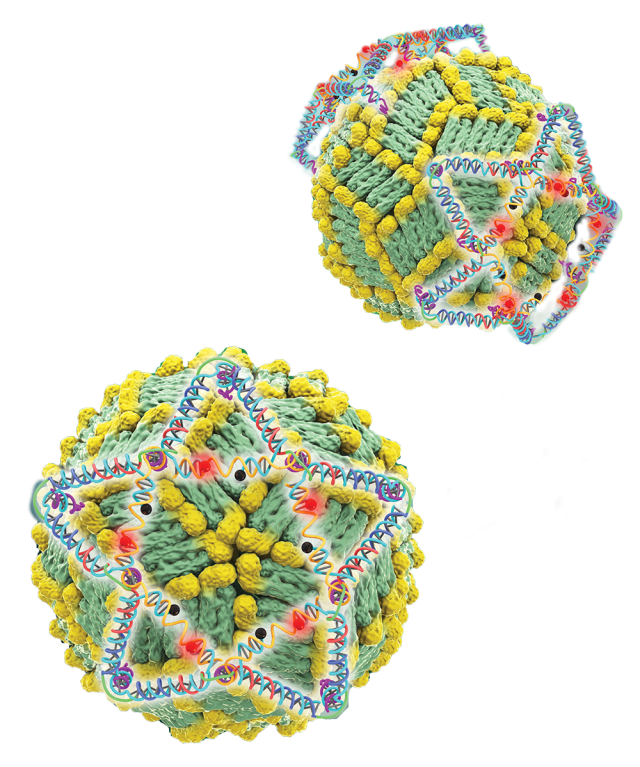
“So, we have something that can be tailored specifically to the coronavirus,” Dordick told the publication FierceBiotechResearch. “There has been very rapid research that has come out in the last couple of months about the proteins on the surface of the coronavirus. Once we know their approximate location on the surface, and what the receptor is on cells that the virus targets, it allows us to very quickly tailor this DNA nanostructure to COVID-19.”
In addition, Dordick and Linhardt are performing tests using heparin, which appears to bind tightly to the SARS-CoV-2 virus that causes COVID-19 disease. This would effectively disable the virus from infecting cells, says Dordick.
Linhardt is a pioneer in the development of the first fully synthetic form of heparin, a commonly used anticoagulant drug. “Because heparin is already a drug, there is a potential for use in this pandemic,” says Dordick.
In a project similar to that of Dordick and Linhardt’s, Chunyu Wang, professor of biological sciences, is looking at screening more than 30 million small molecules for compounds that can specifically bind the SARS-CoV-2 spike protein, and/or disrupt the interaction between it and the ACE2 protein — an essential step for SARS-CoV-2 viral entry and infection.
Dordick’s group is also developing various CRISPR-based detection systems by partnering with a local company that has developed a digital detection tag for biological testing. These platforms, he says, can be used to detect coronavirus and also other viruses in minutes using a handheld device.
“There is already a decent amount of work underway on COVID-19 therapeutic development,” Dordick says. “It’s early stage, and most likely only a few things will be ready to impact the current crisis. But, pandemics will continue, and hopefully some of the work underway can provide routes to solutions down the road.”
Gaetano Montelione, Constellation Chair in Biocomputation and Bioinformatics, and his team have recently posted their computational studies showing 3D structural similarity between a hepatitis C virus (HCV) NS3/4A and SARS-CoV-2 Mpro proteases. Based on these results, they have outlined a priority list of existing drugs that are approved for human use or clinical testing toward HCV NS3/4A and can now be assessed as potential therapeutics for COVID-19.
“Because the development of specific antiviral drugs can take a considerable length of time,” says Montelione, “an important approach is to identify existing drugs already approved for use in humans which could be repurposed as COVID-19 therapeutics.”
Addressing a Supply Shortage
With the world under siege, cascading consequences quickly emerged including supply shortages. This has proven especially problematic within health care, where PPE and ventilators are a matter of life or death, and researchers and students have found ways to tackle this challenge head-on.
Rensselaer engineers Helen Zha and Edmund Palermo were awarded a Rapid Response Research grant from the National Science Foundation to give N95 respirator masks antiviral properties, as well as improve their durability so the masks can be sterilized instead of thrown away after a single use.
“The idea we have in mind is to develop a process where someone in the hospital can apply a very thin coating of an inexpensive polymer material to the mask stock that they already have, that will give it antiviral properties and also enable sterilization procedures,” says Zha, assistant professor of chemical and biological engineering.
Robert Karlicek, director of the Center for Lighting Enabled Systems & Applications (LESA), Mohammed Alnaggar, assistant professor of civil and environmental engineering, and Arunas Tuzikas, LESA senior staff engineer, designed a system using ultraviolet light to quickly disinfect large quantities of masks.
“This particular system is unique because we worked out a process to support the masks vertically,” says Karlicek. “Since UVC radiation is a line-of-sight kind of dose, if there’s any shadow from the mask or anything blocking access to the UVC radiation, you’re not going to disinfect the mask completely.”
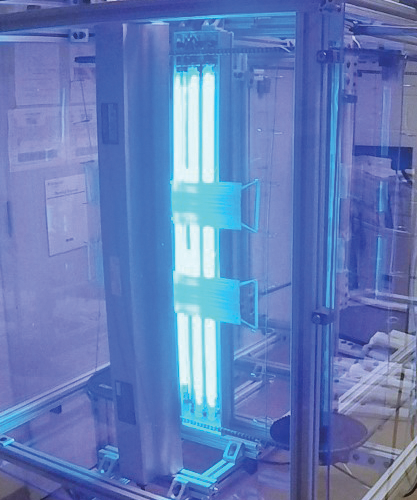
If successful, the system has the potential to help hospitals around the world. “Part of the reason we built it this way was to utilize a rather clean design,” Karlicek says. “It can easily be cloned by just about anybody who wants to build a number of these units.” The system will be set up in New York City at Mount Sinai in May.
“These projects illustrate some of the immediate ways Rensselaer experts have turned their attention to the current crisis and how we are partnering with our clinical collaborators to address COVID-19 challenges,” says Deepak Vashishth, director of the Center for Biotechnology and Interdisciplinary Studies.
Even while social distancing, Rensselaer engineers have found ways to tackle the PPE problem.
“We’re excited to work together, at Rensselaer, at home, and with our industrial partners, to create ingenious solutions,” says Robert Hull, acting vice president for research. “Our work is grounded in fairly simple engineering principles, but it’s going to save lives.”
Hull has been working with manufacturing faculty and staff, along with Industrial Tool & Die Company (ITDC), a Troy, New York-based business, to manufacture face shields for Albany Medical Center. Using six 3D printers from the campus, three from ITDC, and an open source design from Prusa3D, the group has already delivered over 370 face shields to Albany Med.
The group is organizing a larger manufacturing effort with plastic injection molding and laser cutting machines ordinarily used to teach students the elements of manufacturing. Where a 3D printer takes an average of about one and a half hours to produce a single face shield, the plastic injection molding tools at the Manufacturing Innovation Learning Laboratory (MILL) will produce at least 50 face shields per hour. They have also developed a new design that addresses a vulnerability in 3D printed designs, offering more protection for health-care workers.
The Forge, a student-managed makerspace, teamed up with an industrial 3D printer company, Stratasys, in a separate off-campus collaboration to provide equipment to St. Peter’s Health Partners in Albany.
In mid-April, The Forge launched the Off-Campus-Resources Initiative, which is open to any Rensselaer-affiliated individuals. Within days, they had 18 volunteers comprised of current students and alumni. “In the 3D printing community, as soon as we started hearing that there’s a shortage, we said to ourselves, ‘We can make that,’” says Russell Roberts, student leader of The Forge.

“We’re proud of what the students are doing remotely, on their own, and separate from our on-campus efforts,” says Sam Chiappone, director of the MILL.
Jennifer Aspell ’85, president of Bright View Technologies, saw the need for PPE. After developing a face shield prototype, her company recruited 60 unemployed workers to assemble the shields from home and has supplied over 200,000 to officials in North Carolina.
An ocean away in Barcelona, Spain, exchange student Guillermo Lopez-Balcells saw a similar need. While paying for a purchase in a pharmacy, he had to toss his credit card over several benches to the cashier. “They told me, ‘We’re sorry for this but if we don’t have the benches people get too close and it’s dangerous.” Inspired by the incident, Lopez-Bacells used his family’s factory, which had been temporarily closed due to the pandemic, to produce protective screens for essential businesses. They have since sold over 6,000.
The Unknown: Life After COVID-19
As of the printing of this special section, some pandemic epicenters were reporting modest declines in COVID-related hospital admissions, intubations, and deaths. Yet, new hot spots were emerging in communities such as South Dakota, Michigan, and Indiana.
According to economist Vivek Ghosal, the Virginia and Lloyd W. Rittenhouse Professor and head of economics, the impacts of this pandemic to the health-care industry will be game-changing.
“One thing this crisis has proven is that we really need to bring products to market faster. In the biopharmaceutical industry, it is inevitable that they will have to go to more efficient production, more IT use,” he says. “Collaboration among companies will be required to speed up innovation, reduce R&D costs, and increase speed to market.”
The impact to the overall economy will be long-lasting. “People out of work may come back to find a world where companies have learned to do more with IT, remote work, and part-time work.”
In an April 30 report issued by the Center for Infectious Disease Research and Policy, public health experts predict the COVID pandemic will last up to two years, infecting up to 60% of the population.
As the pandemic wages on and the world continues to fight it, the research and breakthroughs from the Rensselaer community will continue to make a difference.
“These challenges have brought out the best in our community. As a community, we always live the Rensselaer spirit of innovation and perseverance,” says President Jackson. “I know that spirit will see us through these challenging times. Life will return to a new normal, but we will emerge stronger, bolder, and more resilient.”
After the spring issue of Rensselaer magazine went to print, we learned of three Rensselaer graduates who are also contributing to a world grappling with COVID-19 and its effects. Ardalyst, a cybersecurity and digital transformation company based in Annapolis, Maryland, is helping as the world becomes increasingly more digital.
Josh O’Sullivan ’01, the company’s co-founder, along with Ray Mendenilla ’01, senior vice president for sales and marketing, and Jessica Lawrence ’02, lead analyst, are working to educate people working from home about cyber risk and help businesses operating remotely develop and implement a robust cybersecurity strategy.
O’Sullivan, Mendenilla, and Lawrence met while attending Rensselaer as part of the Institute’s Reserve Officers’ Training Corps naval science program.
We also learned that Zach Hines ’09 and Ryan Doherty, cofounders of the optics company Ripclear, shifted their business focus as the COVID-19 pandemic started, and began manufacturing personal protective equipment. In just months, Ripclear delivered millions of face shields and face masks to frontline workers in need.
Are you doing work or research to aid in the COVID-19 pandemic? We want to hear from you! Email us at alum.mag@rpi.edu and provide your name, class year, and a summary of how you are helping.